American Black Journal – Mental Health Awareness in the Black Church
May 31, 2022
This Week on American Black Journal:
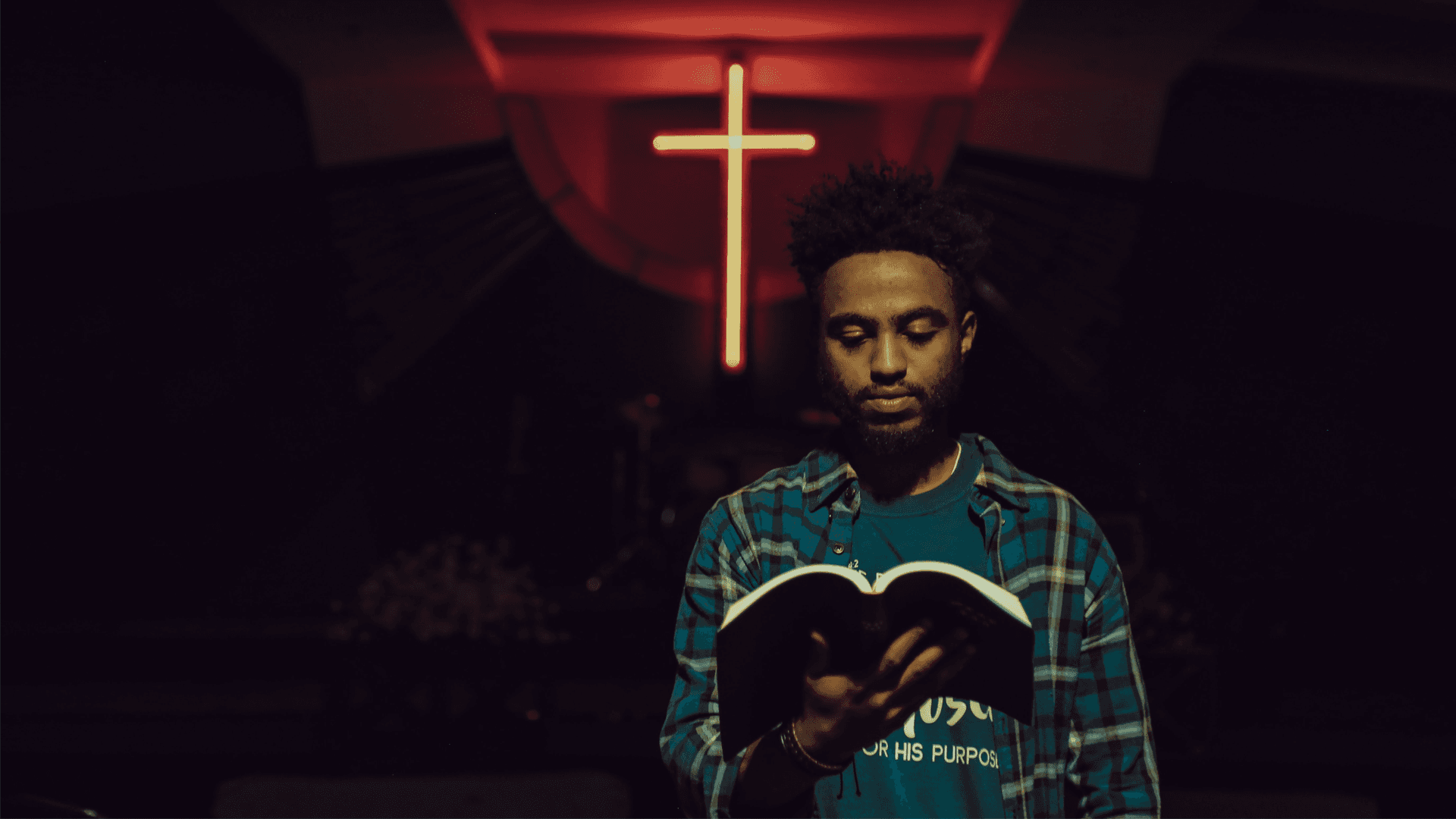
Addressing Mental Health Awareness, Support in the Black Church
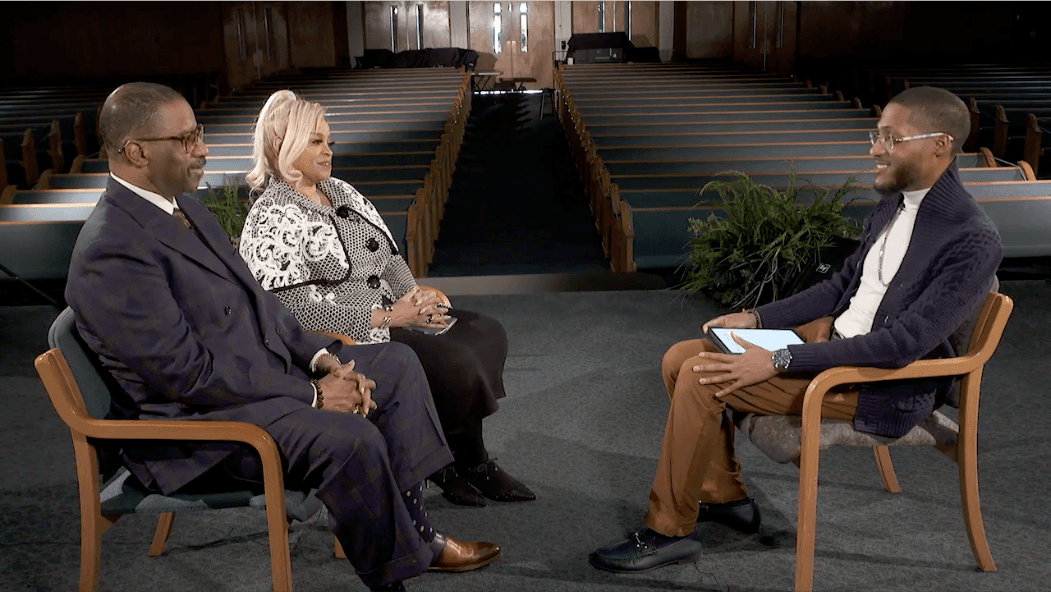
“American Black Journal” continues its “Black Church in Detroit” series with a candid conversation about mental health in the Black church. Guest host Trudy Gallant-Stokes examines the Black church’s role in helping congregants with mental health issues and why it’s important for pastors to practice self-care too.
Rev. Dr. Carla Spight-Mackey, a minister and licensed clinical therapist at Detroit Wayne Integrated Health Network, and Rev. Dr. Tony Henderson, associate professor of practical theology at the Ecumenical Theological Seminary, join Gallant-Stokes for a conversation about how faith intersects with mental health in the Black church, how to reduce the stigma of mental illness in the Black community, and how clergy can maintain good mental health practices themselves.
RELATED: Mental Health Awareness Month Highlights Disparities and Stigma in the Black Community
Plus, the trio discusses the pandemic’s impact on mental health over the past two years and how the religious community has come together to support mental wellness in the Black church during a time that’s been filled with loss, grief, isolation and other mental health challenges.
Watch Now:
[et_pb_video_slider_item admin_title=”Full Episode” src=”https://www.youtube.com/watch?v=qif37psCyhs” _builder_version=”4.17.4″ global_colors_info=”{}” show_image_overlay=”off”]
Full Transcript:
Trudy Gallant-Stokes: Welcome to American Black Journal. I’m Trudy Gallant-Stokes sitting in for Stephen Henderson. We’re continuing our special series on the Black church in Detroit, produced in partnership with the Ecumenical Theological Seminary and the Charles H. Wright Museum of African-American History.
Today, we’re focusing on mental health and the Black church. Historically, stigma has surrounded mental illness in the African-American community, and many rely on faith and prayer instead of seeking professional help. I sat down with the Reverend Dr. Carla Spight Mackey of Detroit Wayne Integrated Health Network, and the Reverend Dr. Tony Henderson from the seminary for a candid conversation about how the Black church can be a vital partner in promoting mental wellness.
Trudy Gallant-Stokes: It’s so great to have both of you with us, particularly during this May mental health month. It’s such a crucial topic, and a topic that really needs to be discussed more, particularly in the Black church and the religious community. So, I don’t know, I thought when I was thinking about self-care, particularly for pastors. You know how when you get on a plane and they tell you that if you have somebody with you, make sure you put your oxygen first before you put on the oxygen of the other person? Do you see that analogy in terms of the need for self-care for pastors so that they can share and help others?
Rev. Dr. Tony Henderson, Associate Professor, Practical Theology, Ecumenical Theological Seminary: Absolutely. I always tell my students that you’ve got to take care of yourself and know the lay of the land before you start trying to help others. Because if you’re sick, you won’t be able to give your best to the process.
And you have to be willing to set boundaries. You have to be honest about your limitations, and you have to learn how to network with people in the environment. Whether that be mental health specialists in the community, at the hospital, social workers, psychiatrists, so forth and so on. So that you can give it your best shot when trying to help, not only yourself, but your parishioners as well.
Trudy Gallant-Stokes: Is this something that’s taught in theology school or is this something that you address?
Rev. Dr. Tony Henderson: Oh, yes, I teach introduction, one of the courses, I teach several courses. For one of the courses that I have been teaching for 18 years that I’ve been on the faculty is “Introduction to Pastoral Care and Counseling.” And it’s a 10-week, we’re on a ten-week quarter basis. And one of those sessions, Dr. Mackey has been through it. She’s one of my former students and one of my distinguished colleagues now.
We teach self-care. And you’ve got to get enough rest, you’ve got to eat properly, you’ve got to exercise, you got to know when to say no and mean it. You’ve got to know how to offer other resources without burning yourself out. And so, you have to set these things up. Nobody can do it for you. And that’s why it’s good to learn the lay of the land. The average pastor can do well with about 100 people. He or she can take care of them with little to no problem. But when it starts to get to be 300, 600, a thousand, 5,000, 10,o00— no one person can take care of all of those people. So you need a team.
Trudy Gallant-Stokes: Absolutely.
Rev. Dr. Tony Henderson: A local team, and you need professional resources in the community upon whom you can call to help. And let your people know there may be a fee involved for accessing these services, because we are trying to make sure that the student, I mean, not the student, but that the potential client and the parishioner gets the best help that he or she, that is available in the community among the .
Trudy Gallant-Stokes: So Dr. Spight-Mackey, are we getting better at it? Are we making progress in terms of being able, knowing the types of help that people need and offering that?
Rev. Dr. Carla Spight-Mackey, Clinical Specialist, Detroit Wayne Integrated Health Network: I think absolutely so. One of the wonderful things that I think is occurring across systems, and I always like to talk across systems, because not only am I fortunate enough to be an ordained minister and associate pastor, but I’m also a licensed clinical therapist. And so, there are many of us who serve in pastoral positions. Counselors, social workers, therapists who work within not only our congregations, but also in our communities.
What is great, I think, that is happening, for several years now, I have served on the faith-based community for Detroit Wayne Integrated Health Care. So we have ministers, I’ll say, ingrained in the services of mental health through committees at Detroit Wayne, the Red Cross, all the way across Wayne County. And so we are serving through prevention and through education, through those who are in ministry capacity across our county. And so it’s totally ingrained and infused, I think, through mental health, through substance abuse services within the church. And many of them local pastors and ministers, servant leaders in the church are a part of that committee.
Trudy Gallant-Stokes: So now we’ve had this additional layer, unfortunately, of the pandemic. I’m sure that that’s probably caused some new challenges that you’ve had to face. So, Dr. Henderson, talk about that and then I’ll come back to you, Dr. Spight-Mackey as well.
Rev. Dr. Tony Henderson: Basically, what many of us has done, as Dr. Spight-Mackey has said, we have networked with various agencies and denominations that do workshop over Zoom that will address, that have addressed rather and are continuing to address, how do we maintain our sanity and a good state of mental health while we’re under this pressure? We have to find ways to find freedom within the boundaries and make the most of it.
I’ve done workshops with the Presbytery of Detroit that sponsored a workshop for men who seemed to have had a lot of trouble with staying in place and still taking care of their families, while in the first stages of the pandemic. There are professors, pastoral care professors and specialists around the country who have developed strategies on how to do this successfully. We all agreed that the main thing is that the person who feels pressure or who is stressed has a real contact, point of contact, with a healthcare professional.
That can be in-person if possible, but that can be by phone if possible. That can be by Skype on a computer, that can be by Zoom and many other platforms that we use. We try to use the no-cost platforms first, because a lot of people don’t have the extra financial resources that would lead them to have to pay. And then we talk with pastors about mimicking the same thing or duplicating the same processes and procedures when dealing with their sick folks.
My own wife had a double bypass open heart surgery, April 27th of last year. I couldn’t even go to the hospital to see her. I had to check on her and talk with the surgeon by phone. systems checked on me by phone and by Zoom. They set up a situation. One of my preacher friends, and pastor friends, helped me, introduced me to this system. I’d never get the name of it right, but you create your grocery list, you get it to somebody who’s familiar with that service. They pay somebody to go do the shopping and they deliver your groceries at your front door.
And so, for about 6 to 9 weeks, during her year-long recovery, that’s how we got our groceries until the doctor freed her to be able to walk and go to the grocery store. So there are, and we transferred that and shared that with our church members and with other pastors.
Trudy Gallant-Stokes: So, Reverend Dr. Spight-Mackey, as Dr. Henderson said, there are luckily a lot of services out there and a lot of services that have developed since the pandemic. What approaches have you found to be most successful, or what new things have helped since we have been in this very unique time?
Rev. Dr. Carla Spight-Mackey: Well, one of the great things that has occurred is telemedicine. Telehealth. That was instituted in Detroit Wayne Integrated Health Care System. It was integrated right at the front end of the pandemic so that people could still contact a therapist. That they could still, you know, therapy could come straight into your computer or straight into your phone. And so that that has been ongoing.
We have crisis services. We actually also have a COVID residential. So if somebody has COVID, they can still receive services through Detroit Wayne, because they’re, you know, we have providers who have made themselves available to have places where members can quarantine and still receive services. So, I think that the systems have come together well.
When we talk about, you know, the church and mental health, that we have many of our churches who have opened their doors and are opening their doors and their systems to be available. And so many ministers, as Dr. Henderson was saying, you know, a lot of ministers are in seminary taking classes in mental health. You know, they’re taking classes in counseling, in mental health.
So we have I would, I won’t say it’s a brand new phenomenon. I say, it’s an increased opportunity where many ministers are learning more in-depth knowledge around mental health, as well as recognizing, as Dr. Henderson started out, you know, you’ve got to put on the oxygen mask first. You just can’t run out here and say, you know, “I know how to take care of this.” Because the level of trauma and the level of health issues that we are dealing with and seeing on the front line are astronomically more than when I came into the field, and I’m gonna say in the seventies cause, you know, I’m just that young.
Trudy Gallant-Stokes: That’s our little secret. But I think that you touched on something that is probably going to continue because it has been a good thing. The availability of telehealth and the ability to have Zoom, because sometimes people don’t have transportation or there are other issues. And so at least some of these challenges are now being addressed.
Still, the big picture, and it looks like we’re finally chipping away at that, is about the Black church. And historically, there’s been somewhat of a stigma against seeking out mental health services. So how have things changed? And, you know, you have some people like, “Hey, I can just pray this away, it’s going to be okay.” But, I know that both things can work and work beautifully, but doesn’t mean that one thing has to exclude the other.
Rev. Dr. Carla Spight-Mackey: No. I think we have to be honest to say, and I hear it more often now, “Okay, we gonna pray and then you can go see the therapist. Here’s a list of therapists that are available for you to talk to.” Because, yes, we need to pray. Yes, we need to hold strong to our faith. But we ought to also recognize that each of us, because we walk into ministry, because we love God, does not mean that we have all the tools necessary. And that’s why God allows some of us to become licensed professionals.
That we can partner with licensed professionals to get the help that everybody can get the help that they need by somebody who has been trained to address those issues. I think we have to, that’s where we have to stay. That’s what we have to hold on to. That there is more than one of us available, and many of us now have been trained to help those who have a worse situation than we do.
Trudy Gallant-Stokes: Reverend Dr. Henderson, what do you say to people when they say, “I don’t need to see any counselor, you know, Lord’s going to take care of me if I just pray, I’m going to be all right.” What do you say to people when they say that to you?
Rev. Dr. Tony Henderson: I let them know that while prayer is good, prayer is not an end-all. And we must see the therapists and the specialists as ministers as well. I take an African mindset and approach. I don’t distinguish between, unless I have to, between the sacred and the secular. It’s just as important for you to take for a person who needs medication and therapy to do that. As it is to spend 30 minutes to an hour in prayer.
It’s just as important for them to go away on a retreat and spend time where that therapist and give specialized time. And use models of health that can help them face their situation, figure out a way to deal with their situation and cope with it. And I let them know you may not ever get over whatever it is that troubles you, but you can learn to live with it without it halting you and halting the progress in your life. And so we take a holistic approach.
And, see, the other advantage we have Miss Stokes, is that we have specialists like Dr. Spight-Mackey and others who are in mental health as licensed practitioners. They have one foot in the church and they got one foot in the field. And so they see people on both sides and can properly recommend what should be done for that person’s improvement. We encourage professionals to take vacations, honor your off-day. Take vacations. Go to retreat. See your therapist. You must have, you gonna be in ministry you need somebody with whom you can debrief and talk to every now and then. I don’t care if it’s once a week, once a month. I don’t care if it’s every 3 to 6 months. You got to have somebody. You can’t carry this stuff, it’ll kill you. It’ll cause you to kill yourself.
Trudy Gallant-Stokes: Yes. And unfortunately, another area because of COVID and all the tremendous loss that’s taken place over the last two years. Grief counseling and families who have lost family members, children who have lost parents. Dr. Spight-Mackey, what are some services or you know, sometimes people don’t even realize when, you know, that they’re having a difficult time coping with the grief. How do you direct them? How do other family members kind of direct the person and encourage them to get into therapy?
Rev. Dr. Carla Spight-Mackey: Interesting you picked on me.
Rev. Dr. Tony Henderson: I got your back.
Rev. Dr. Carla Spight-Mackey: At the very beginning of COVID, I was fortunate to find an organization called Grief Share. Grief Share is a grief support group that you don’t have to be trained, because we join the group because we are going through that process. But it is a guided process through Grief Share and lots of support that happens through Grief Share.
But, we have to let people know grief is normal and people are going to say all kinds of things like, “You need to get over it.” Like, you know, you broke a cup. No, you need to be able to allow that to happen. I always say things, and people look at me kind of strange when I say it, “If God didn’t want you to cry, he would not have given you tear ducts.”
Rev. Dr. Tony Henderson: Amen.
Rev. Dr. Carla Spight-Mackey: So you need to go ahead and cry, you need to allow people to have the feelings that they have, but also to give them that hope, you know. That one day, one day the tears will slow down and you’ll see a smile coming back. One day. But I’m not one to try to tell you when that day is. I can just say one day.
Rev. Dr. Tony Henderson: That’s right, that’s right.
Rev. Dr. Carla Spight-Mackey: Grief is a personal, individual process. And to allow, to be allowed to be inside that grief process with somebody is a huge honor. I have stood at the bedside of my mother dying. My sister died. My brother died. Some of my, my one sister who I spend one day a week with, that I stood with her on the telephone. Because I was relating, when Dr. Henderson talked about his wife being in surgery, I was on the phone when my sister was in emergency with her husband dying of COVID. And we stayed on the phone. She said, “Well, we can hang up now.”
I’m like, “I’m not hanging up the phone. You go, you can cry. You can do whatever you need to do. But I’m not hanging up the phone until you say that you’re home and you’re safe because this is something you’re going to go through. And there’s nothing that I can do to stop it. But I can stay. I can be on this phone and give you encouragement as you go through it.” We have to be ready to encourage those who are going through grief and to let them know that this is a normal process. And one day, you’ll find the joy and the healing.
Trudy Gallant-Stokes: I was steered to ask you that question, but Dr. Henderson, anything that you’d like to add to that? Because that is just so crucial.
Rev. Dr. Tony Henderson: I applaud my colleague for her frankness. It’s just beautiful. We have sanitized the grieving process here in America so much until we think it is abnormal for people to cry. And we are even more terrible when it comes to males. If you and Dr. Mackey started crying right now, everybody near you’d know what to do. I start crying and boo-hooing and nobody knows what to do. They think, “Oh, my God, the world’s coming to an end. That man is crying. He’s supposed to be strong.”
And so I have spent time working with African-American males through Sinai Grace Hospital on grief, and letting them know it’s okay to grieve. It’s okay to cry. If you cry, you won’t shoot somebody. If you cry, you won’t stab somebody. If you cry, you won’t rob somebody. You won’t go to prison and you won’t get killed, because you were not allowed to grieve. We have forgotten how to just be with folks. Be with each other. We feel, some of us feel like we got to speak up for God. God’s been talking longer than I am old and will still be talking after I’m gone. And God is old enough, God can speak for God’s self. So we need to learn to not speak for God in moments of grief. It’s a sacred time. Be quiet and be there.
Trudy Gallant-Stokes: Absolutely. We’re getting into our last couple of minutes. So I want to just wind down, but I also want to highlight any other particular services like that. I think that that’s wonderful. The one that Dr. Spight-Mackey mentioned about the grief circle and assisting everyone, and then this program you mentioned at Sinai Hospital. So what other success stories, what other things that you want to promote that people understand that there is help out there?
Rev. Dr. Carla Spight-Mackey: You know, I want to share that Detroit Wayne Integrated Health Network has a crisis line. It’s 24 hours, seven days a week. And that number is 800-241-4949. Twenty-four hours a day and seven days a week. You can call that number and get help. There’s the suicide prevention helpline. They’re all kinds of help. And as a community of Black folk, we need to be okay that we can pick up the number and dial. Nobody needs to know your name, but if you need to talk to somebody, don’t let anybody tell you, you shouldn’t be talking. You should talk as much as you feel like talking.
Rev. Dr. Tony Henderson: That’s right.
Trudy Gallant-Stokes: Thank you both so much for joining us today. And yeah, I think that’s the main thing. As long as people remember that help is out there and particularly in the Black community, there are many resources that people can take advantage of and really make a difference. So thank you both so much for joining us today. And much success in the future.
Rev. Dr. Carla Spight-Mackey: Thank you for having us.
Rev. Dr. Tony Henderson: Thank you for having us.
Stay Connected:
Subscribe to Detroit PBS YouTube Channel & Don’t miss American Black Journal on Tuesday at 7:30 p.m and Sunday at 9:30 a.m. on Detroit PBS, WTVS-Channel 56.
Catch the daily conversations on our website, Facebook, Twitter and Instagram @amblackjournal.
View Past Episodes >
Watch American Black Journal on Tuesday at 7:30 p.m. and Sunday at 9:30 a.m. on Detroit Public TV, WTVS-Channel 56.
Stay Connected
Subscribe to Detroit PBS YouTube Channel & Don’t miss American Black Journal on Tuesday at 7:30 p.m. and Sunday at 9:30 a.m. on Detroit PBS, WTVS-Channel 56.
Catch the daily conversations on our website, Facebook, Twitter, and Instagram @amblackjournal.
Related Posts
Leave a Reply
Your email address will not be published. Required fields are marked*