Caregiving and mental health: ‘Overload in every sense of the word’
May 26, 2023
By Scott Scanlon, The Buffalo News
Claudia Holewinski was still in high school when she and her 24-year-old sister became caregivers after their mom was diagnosed with leukemia.
Darcy Thiel helped care for her mother and husband, who both died from cancer, and later her father, who succumbed after eight years to complications from Parkinson’s disease.
Angela McIntyre, a nurse who cares for vulnerable patients, soldiered through a tough job before the pandemic made it a heavier lift.
All these women have found the physical demands of caregiving a challenge.
The mental pressures?
“You’re on overload in every sense of the word,” said Thiel, a mental health counselor in Buffalo. “You’re coping with all of these in-the-moment things, but you also know you’re losing your person. That never leaves your mind.”

That pressure has become more common. AARP estimates the number of unpaid caregivers – roughly one of every five adults – has grown nearly 25% during the last half-decade, to about 50 million people. They spend an average of 24 hours a week with hands-on care and managing housework, finances and transportation for a family member or friend with a serious illness, developmental disorder or disability.
Many juggle employment and almost all limit time for self-care as they struggle to navigate a complex and overburdened healthcare system, according to caregiving advocacy groups.
There are angels in health care, Thiel said, “but when I tell caregivers, ‘Hey, listen, we need to be well educated because our medical system is kind of a disaster,’ Nobody goes, ‘Oh, no, we found it to be completely helpful.’”
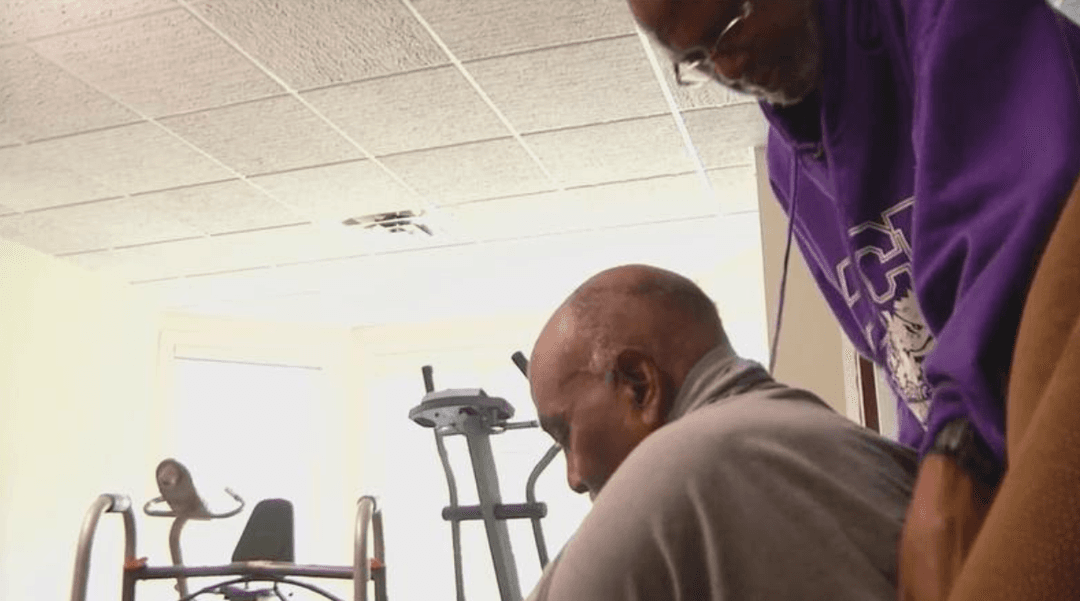
Those angels include many of the 4.5 million paid caregivers in the United States who work in private homes, residential care, nursing homes and hospitals, a number expected to grow by 1 million more within five years. Compassion fatigue was always a danger. It grew worse with the pandemic.
“I wanted to be there for people in their hardest moments,” said McIntyre, a registered nurse at Ascension Borgess-Pipp Hospital in Plainwell, Mich. “But sometimes they die, and that can take its toll.”
The American Society on Aging also estimates there are more than five million caregivers under age 18 supporting a parent, grandparent, sibling, spouse or friend. That included Holewinski, of Kalamazoo, who was 16 when her mother fell ill.
“I was just anxious all the time,” she said, unsure of how her mother’s illness would progress and what that would look like, but also conscious of putting on a brave front for her mother.
“I didn’t want her to feel worse,” Holewinski said, “and I knew she already felt bad.”
An emotional toll
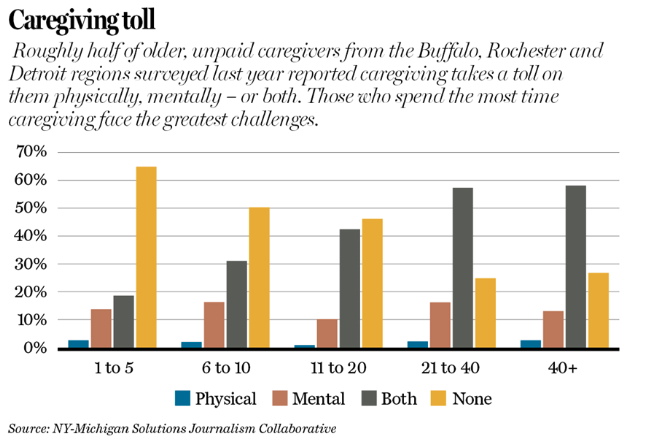
Roughly half of 1,000 unpaid caregivers surveyed last year in the Buffalo, Rochester and Detroit regions said physical and mental health challenges came with their roles. The more hours spent caregiving, the greater those burdens. The same held true for the youngest, least educated and lowest wage earners, according to the survey, commissioned by the New York-Michigan Solutions Journalism Collaborative.
The findings followed a 2021 report in the New England Journal of Medicine that found symptoms of anxiety and depression were a serious problem for more than one-third of unpaid caregivers in Massachusetts and a moderate problem for another 51%.
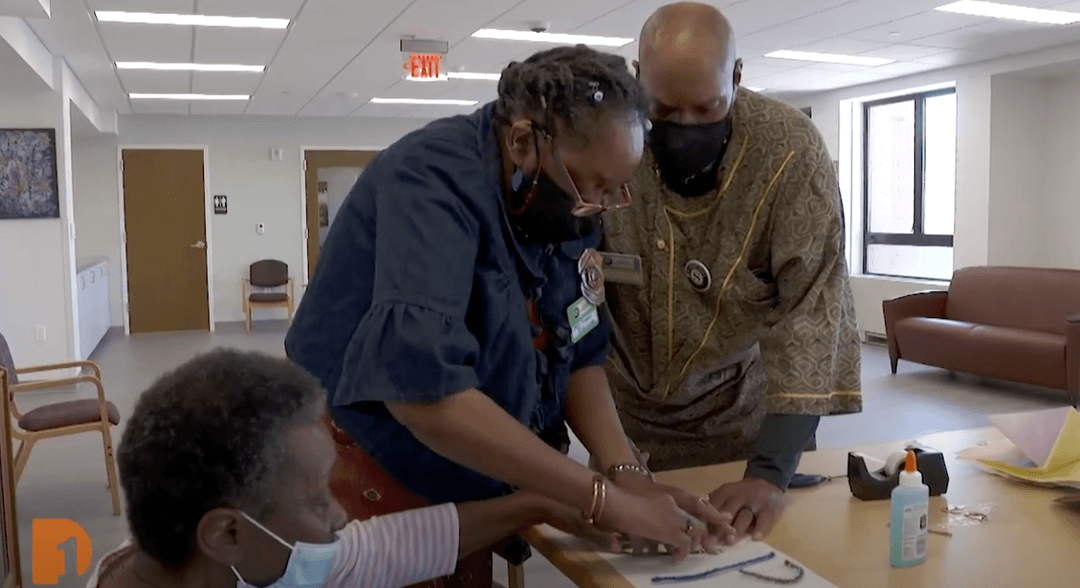
Researchers who issued the report called on healthcare providers to recognize the important role caregivers play as part of a medical care team. They urged providers to help find better ways to help caregivers connect with respite services and other resources to buttress their mental and emotional well-being.
Paid caregivers face daunting challenges of their own. One in three doctors, physician assistants and nurses in an American Medical Association survey during the last half of 2020 said they wanted to reduce their hours. One in five physicians and two in five nurses wanted to leave their jobs. In a related survey the following year, the most common reason nurses gave for planning to leave was because of the way work affected their health and well-being. The second most common reason was insufficient staffing.
“During Covid, we weren’t always able to get to everyone in time, and that was horrible,” said Kelly Asselmeier, a nurse who works with McIntyre. “It could be overwhelming, and we would call on the emergency department nurses to help, but we could still fall behind. We love our work, but that was hard.”
Caregiving and work
“A National Survey of Caregiver Stress in the U.S. Workforce,” released in fall 2021 by the Rosalynn Carter Institute for Caregivers, reported the emotional stress of handling both a job and caregiving responsibilities was the biggest challenge.
That is no surprise to Thiel, whose caregiving journey started with her mom, Vera, who died three weeks after being diagnosed with late-stage colon cancer in 2007.
Thiel posed lots of questions to health providers as her mother’s health deteriorated. She backed down at first on treatment decisions, she said, “because I’m not a doctor.” After a tough conference call involving her mother’s primary care physician, it was decided that hospital-based hospice was the best option because Vera Thiel was too sick to leave. She died four hours after it started.
“It was the only four hours she didn’t suffer,” Darcy Thiel said.
Her siblings learned during the process that her sister Lisa provided the best hands-on care and Thiel was the best advocate, despite her inexperience.
Three years later, Thiel became a primary caregiver when her husband’s routine gallbladder surgery revealed a large tumor, which turned out to be cancerous. The doctor left the operating room, seeking her consent to either remove it or take a biopsy and leave it in. Her intuition told her the tumor should come out. She asked the surgeon what he would do if her husband was one of his loved ones. He said he’d get a biopsy, because recovery would be so taxing that it could delay cancer treatment and most likely shorten his life.

“The weight of the world is suddenly on your shoulders,” Thiel said, “and you’re not equipped.”
Learning as you go
Thiel and her husband, Tim Colvin, an engineer, were told he had one to two years to live, so both chose to keep working.
They also made a key decision: Accept help offered by family, friends, fellow church members and strangers.
“When we did that, it was enormously helpful for our own mental health and emotional health,” Thiel said. “The people in our lives told us we helped other people and they asked us not to rob them of the opportunity. They helped us with just about everything.
They walked our dog, they provided meals, they went shopping. They cleaned our house, they transported our son, they did research for us.”
That support allowed Thiel to arrange and keep track of her husband’s growing number of medical appointments; learn what medications, foods and activities could support his health; and handle the abundant paperwork that goes into cancer treatment and end-of-life care.
The support team and resilience were vital, as Colvin took a turn for the worse three months after his diagnosis. He died 10 weeks later, leaving three adult children from a previous marriage along with Thiel and their 8-year-old son, David Thiel-Colvin.
The caregiving journey, including the tighter bond she forged with her husband during his last months, inspired Thiel to write a book, “Bitter and Sweet: A Family’s Journey with Cancer.”
“I don’t know how people do this for years,” she said as she remembered those days. Statistics show caregivers are more accident-prone, she said, and more likely to get sick themselves.
Protracted caregiving
Thiel came better prepared to manage protracted caregiving for her father, David, a General Motors retiree diagnosed with Parkinson’s disease in 2010.
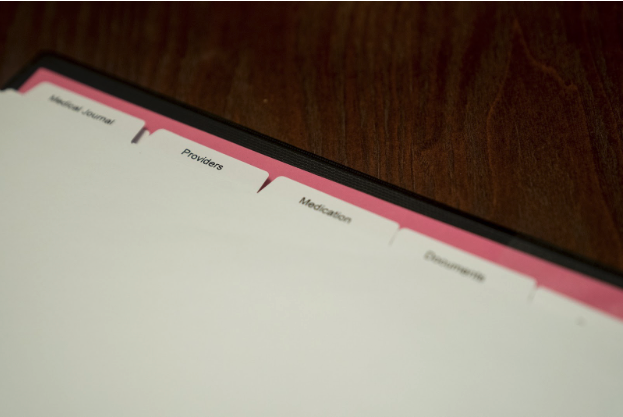
He agreed to move into assisted living in 2017, as his health worsened and it became too hard to live on his own. By that time, Thiel had improved the kind of notebook she started when her husband was sick. It included end-of-life plans that included a living will, health care proxy, power of attorney, Medical Orders for Life-Sustaining Treatment and Do Not Resuscitate order.

David Thiel was exhausted and in pain when he got his last urinary tract infection and decided he would pass on an antibiotic. An emergency room doctor who talked with him and his daughter supported the decision, Thiel said, but the assisted living staff pushed back.
“Their doctor came to the apartment to see Dad and literally was bullying him,” she recalled.
Thiel filed a complaint with the State Department of Health to stop the harassment. Her father died in August 2018, at age 86.
Roadblocks and solutions
Two years ago, Thiel launched the Resilient Caregiver’s Lifeline, a self-paced online support program that bubbled out of her counseling practice during the pandemic.
She helps those who enroll compile a binder that includes sections for medical and real estate information, treatment and end-of-life directives, and how to sell homes, declutter and downsize.
That kind of organization is key for caregivers because it makes it easier to communicate with healthcare providers and a support team, as well as advocate for those in their care.
Support groups with fellow caregivers are also important, she said. Her program includes two weekly online group sessions in which participants can interact with caregivers from across the country. It also provides access to a private Facebook page with tips and short informational videos for caregivers.
Throughout her caregiving experiences, Theil regularly visited a mental health counselor –- and continues to do so as part of her self-care.
McIntyre, the registered nurse in Michigan, does the same each week as part of her workplace benefits.
“I do it on video, right from my couch with my cup of coffee,” she said. “My therapist is cool because she understands caregiver burnout.”
This and other self-care may bring on some guilt, Thiel said, but she advises caregivers to do it anyway, because it brings perspective and revitalization.
Thiel can arrange a free 15-minute consult for her program for those who visit marriageandfamilycounseling.net. It runs six months. It isn’t for everyone. The cost is $1,500 to $2,000, which Thiel considers an investment in a journey that can become much more expensive.
Thiel has worked closely with two dozen caregivers who chose to take the program and traded text messages and emails with more than 300 others, providing tips and encouragement. Those who decide not to participate in the program say the cost in time and money are the biggest barriers. The program also is open only to those who speak English.
Marla Elrod, of Nuevo, California, signed up for the program last April, five months after her 90-year-old father fell and broke his hip – and a hospital and health insurance company placed him in a rehab center of their choosing without consulting his family.
“About the time I connected with Darcy, I was mentally and physically drained,” Elrod said. “Working full time, talking with him daily, sometimes more than once, and visiting as much as possible. I took all the calls from the assisted living facility, doctors and physical therapy as well as getting him to and from all appointments. That required arranging medical transport because … I wasn’t physically able to move him and put his wheelchair in the car.”
Talking with Thiel and other caregivers who understood the circumstances made things more manageable, as did the caregiving notebook. It was key to her decision to start hospice care after her father was hospitalized July 5 with fluid on his lungs, surgery was considered and Elrod asked doctors the right questions about its potential risks and benefits. Her father died three days later.
“The whole experience would have been much less stressful if I had Darcy’s input earlier,” Elrod said.
A lot of those who use her program care for someone with dementia. Many also turn to author Teepa Snow and her Positive Approach to Care online program. Snow, a dementia care consultant and educator, offers online programs for a cost and free tips on her YouTube channel.
Other resources are available free, though many who enter caregiving aren’t sure where to look, especially as illnesses and needs progress.
RELATED: Resources to help caregivers
County Offices of Aging, regional chapters of the Alzheimer’s Association and the Caregiver Action Network can be a good place to start.
AARP can provide valuable tips, as well as Trualta, an online platform for family caregivers available free for all New Yorkers through the state Department of Health and in several Michigan counties through senior services programs.
Paid caregivers can usually find support through workplace programs, some of the tools unpaid caregivers use and the Dr. Lorna Breen Heroes’ Foundation, which provides solutions and resources for healthcare workers and facilities where burnout is common.
The bottom line
Thiel tells prospective caregiving lifeline clients that her program can provide greater assurance, balance and meaning. She underlines that caregiving will still be the hardest thing they’ve experienced – including when it’s over.
She has learned there is no quick fix, magic bullet or mountaintop revelation to protect and preserve a caregiver’s mental health. Acceptance, she said, does the most to lighten the load.
“I try to help people distinguish between feeling guilty and feeling badly,” she said. “Guilt is a healthy emotion, when it’s appropriate. It’s our moral compass. But there’s a lot in life that we have inappropriate guilt for, and it helps caregivers to change their narrative…
“You need to accept that your loved one is going to die – not necessarily because of this illness, not maybe for a long time – but to really grapple with mortality,” she said.
“Whatever mentally, spiritually and emotionally you need to do to come to terms with that, you are going to exponentially be able to help your person so much better. It clears up what you need to make decisions and help them make that journey.”
Freelance writers Zinta Aistars and Julie Mack of the Southwest Michigan Solutions Journalism Collaborative contributed to this story.
About This Story:
This article is part of Overloaded and (Often) Unpaid, a joint solutions journalism project on caregiving and mental wellness between the Southwest Michigan Journalism Collaborative and the New York and Michigan Solutions Journalism Collaborative, a partnership of news and community organizations dedicated to rigorous and compelling reporting about successful responses to social problems. The groups are supported by the Solutions Journalism Network.
More coverage:
- Caregivers and mental health: ‘You’re on overload’
- Young caregivers need more support. There’s an app for that.
- A cost-effective alternative to nursing homes
- Paid caregiver burnout: How employers can support workers’ mental health
- Resources to help caregivers
Stay Connected:
Subscribe to One Detroit’s YouTube Channel & Don’t miss One Detroit Mondays and Thursdays at 7:30 p.m. on Detroit PBS, WTVS-Channel 56.
Catch the daily conversations on our website, Facebook, Twitter @DPTVOneDetroit, and Instagram @One.Detroit
View Past Episodes >
Watch One Detroit every Monday and Thursday at 7:30 p.m. ET on Detroit Public TV on Detroit Public TV, WTVS-Channel 56.
Stay Connected
Subscribe to One Detroit’s YouTube Channel.
Catch the daily conversations on our website, Facebook, Twitter, and Instagram @detroitperforms
Related Posts
Leave a Reply
Your email address will not be published. Required fields are marked*